Diabetes and diabetic Retinopathy go hand in hand because diabetic Retinopathy is a problem that can happen when you have diabetes. Diabetes can damage the blood vessels Retina in the back of the eye. This is called diabetic Retinopathy.
Diabetic Retinopathy is a possible side effect of diabetes. It is caused by damage to the blood vessels in the Retina. As a light-sensitive membrane, Retina is responsible for imaging formation and connected to the brain via the optic nerve. The Retina comprises millions of photoreceptor cells, which are sensitive to light. These cells turn light into electrical signals that are sent to the brain. This lets you see.
High blood sugar levels caused by diabetes can cause harm retinal blood vessels making your Vision vulnerable to several diseases. At the earlier stages of diabetic Retinopathy, the blood vessels in the Retina may leak fluid or blood, making Vision blurry or distorted. In addition, damage to blood vessels can cause them to close off over time, leading to the growth of new, abnormal blood vessels. These blood vessels can also leak or bleed, which hurts the Retina even more and could cause vision loss or even blindness.
Symptoms of diabetic Retinopathy
The symptoms of diabetic Retinopathy may vary depending on the severity of the condition. However, Some common symptoms include the following:
- Colours appear faded or washed out
- Sudden decreases in Vision
- Blurred or distorted Vision
- Floaters or spots in your Vision
- Dark or empty areas in your Vision
- Difficulty seeing at night
Diagnosis of Diabetic Retinopathy
Diagnosing diabetic Retinopathy requires an eye doctor will conduct a complete eye examination, including a dilated eye exam, to see if there are any signs of damage to the Retina. They may also use imaging tests, like optical coherence tomography (OCT), to see the Retina and its blood vessels in great detail.
If you have changes in your Vision or have been told you have diabetes, you should see an eye doctor regularly to catch any problems early.
Diabetic Retinopathy treatment
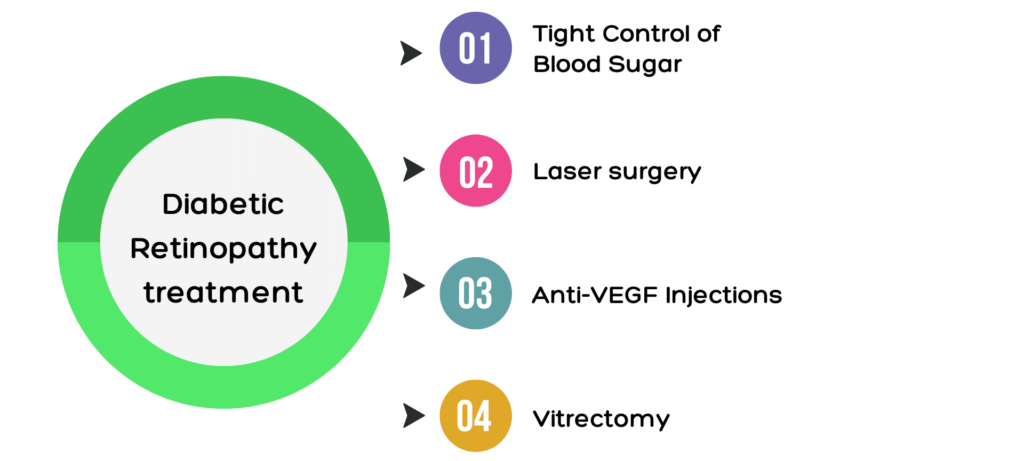
Treatment for diabetic Retinopathy is directly related to the stage and severity of the disease. However, here are some common ways to treat the problem:
- Tight Control of Blood Sugar: The best way to stop or slow the progress of diabetic Retinopathy is to control your blood sugar levels strictly.
- Laser surgery: Laser surgery is used in the treatment of both diabetic macular edema and proliferative diabetic Retinopathy. The laser makes minor burns that stop blood vessels from leaking and slow the growth of blood vessels that don’t work right.
- Anti-VEGF Injections: These medicines are injected into the eye to stop the effects of vascular endothelial growth factor (VEGF). This substance makes abnormal blood vessels grow in the Retina.
- Vitrectomy: People with advanced diabetic Retinopathy may need a surgery called vitrectomy. The vitreous gel is sucked out from the eye during this surgery, and a clear solution is injected as a substitute.
Can Diabetic Retinopathy be reversed
Diabetic Retinopathy can’t be cured. However, certain specific treatments can help slow or stop it from worsening and, in some cases, even help improve Vision.
Some options for treatment are:
The strict control of blood sugar: the more you keep your blood sugar level under control, can lower the chance that the blood vessels in the Retina will be hurt even more.
Laser treatment: With laser therapy, abnormal blood vessels in the Retina can be shrunk, which stops more bleeding.
Injections: Putting medicine into the eye through an injection can help reduce swelling and inflammation and stop new blood vessels from growing.
Surgery: Surgery may be needed to remove scar tissue or blood from the eye in advanced cases of diabetic Retinopathy.


